
Close


In a time where handshakes are discouraged and physical proximity is avoided, the onus is on the HCA team to circumvent these challenges, while ensuring that quality of care is not compromised.
In response to strict safe distancing measures, HCA kick-started the video consultation initiative in late April. “The overarching aim for video consultations is to provide a cost-effective supplement to home visits, without compromising on quality of care,” explains HCA Nurse Educator Amy Lim, who is also part of the Digitalisation Transformation Team (DTT) responsible for the initiative.
The pandemic has created a unique set of challenges for HCA’s home hospice service model, which entails multiple home visits each day in various uncontrolled environments.
Video consultations are a viable alternative mode of care for some patient groups, to minimise the risk of cross-contamination. To ensure the maximal benefit of the initiative, the DTT developed a comprehensive set of guidelines, which include overarching principles, inclusion and exclusion criteria, documentation processes and risk management protocols.
The inclusion criteria extend to routine check-ins with stable patients and their caregivers, follow-up consultations after a recent home visit, supportive counselling for stable patients and their families, previously unreachable patients and their caregivers. “Some patients are worried that we might unknowingly be carriers of the COVID-19 virus,” Amy explains. “Video consultations enable possible continuity of care in these cases.”
To minimise risk during video consultations, the staff member has to be especially mindful of risk factors, such as falls or injuries and gently remind the patient and their caregiver to be seated or lying down comfortably. They should also check to see if any others are present, to ensure privacy and confidentiality.

The DTT team, comprising Amy (far right), Dr Jasvin Lee (right, in blue) and Research and Bereavement Executive Yeo Zhi Zheng (not pictured) at a training session.
The DTT runs training for all members of the clinical team, to ensure that everyone is on the same page and equipped with the requisite skills to conduct a video consultation. “We sit in for every nurse and clinician’s first video consultation and provide feedback afterwards,” Amy says. “We will also be appointing and training a ‘champion’ in each satellite, so that they can step up and take the lead.”
While the idea of video consultations, on first thought, may seem a little lacking in the human touch, sincerity and compassion are often felt through both words and body language. “I think it’s about how you engage the patient and their family, how you present yourself,” Amy shares.
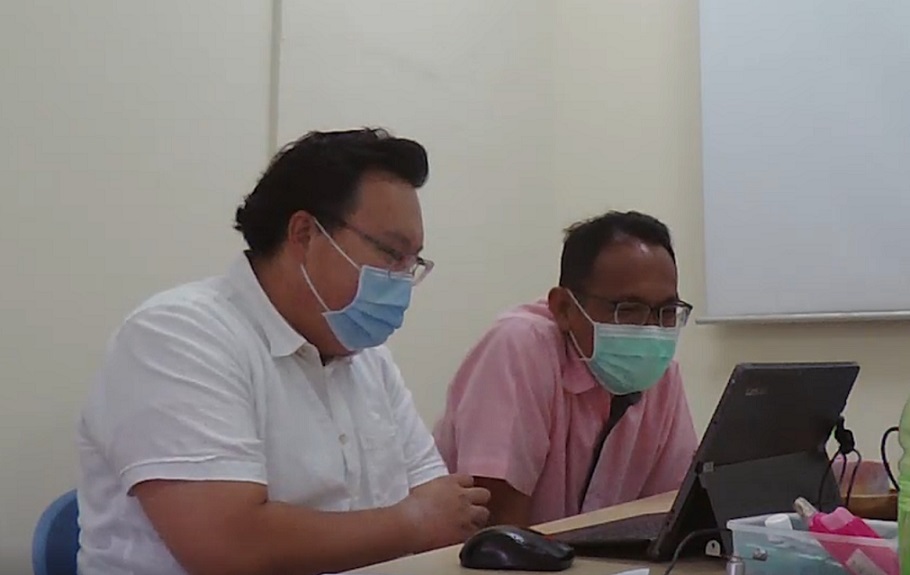
Dr Keson Tay and Nurse Rahmat conducting a video consultation together.
There are undoubtedly limitations to video consultations though. “We cannot conduct physical assessments, such as listening to the lungs,” Amy says. “When it comes to examination of medical equipment such as urinary catheters, it can be awkward and uncomfortable for the patient.”
At present, the clinical team has attended to more than 100 patients via video consultation. While the tides of the pandemic may recede eventually, video consultations are here to stay, as a cost-effective and efficient way of reaching out to those under our care.